Health insurers in multiple states could increase rates sharply on the Obamacare exchanges for 2019, with premiums in Maryland’s individual market set to jump as much as 91 percent.
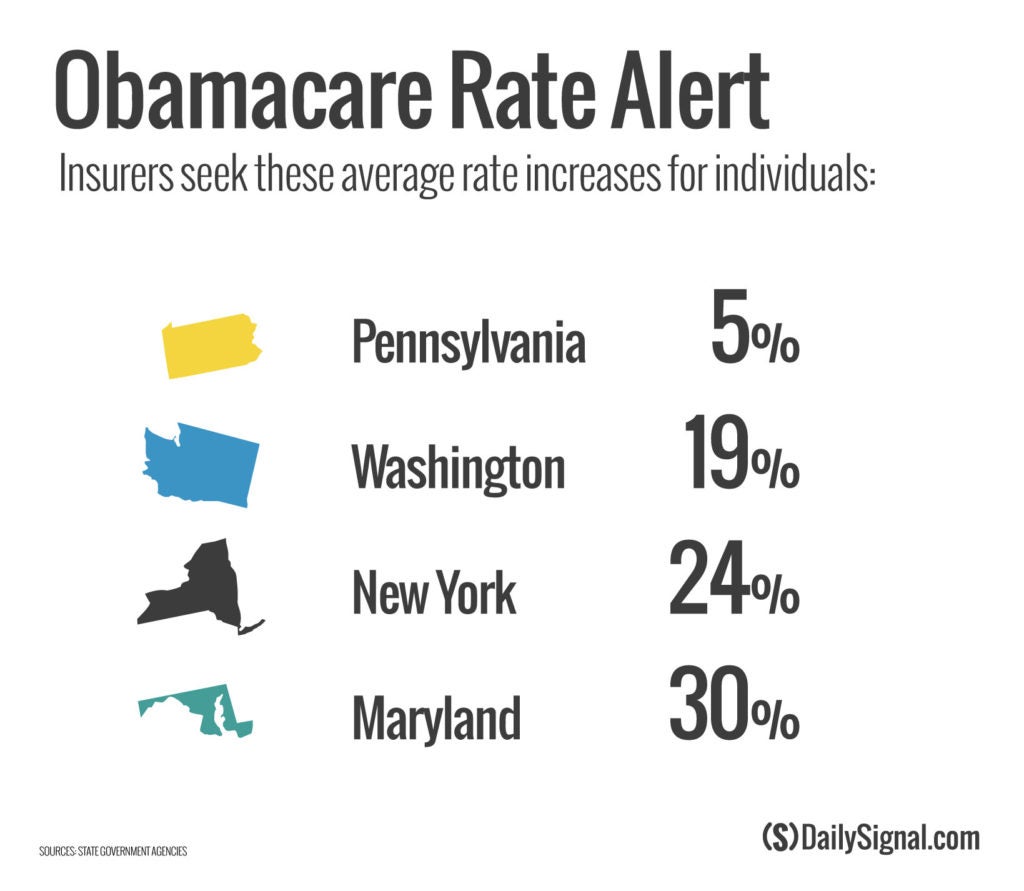
Insurers seek to charge higher Obamacare insurance premiums, proposing average increases in the individual market of 30 percent in Maryland, 24 percent in New York, and 19 percent in Washington state.
By comparison, the average rate hike of nearly 5 percent sought in Pennsylvania’s individual market under the Affordable Care Act would be peanuts.
The Daily Signal depends on the support of readers like you. Donate now
“It is clear in this that what the ACA has done is created through regulations and subsidies basically a high-risk pool in the individual market,” Ed Haislmaier, senior research fellow in domestic policy studies at The Heritage Foundation, told The Daily Signal in an interview.
In Maryland, CareFirst requests an increase of 91 percent for a plan currently covering 15,000 residents.
Maryland and other states blame congressional Republicans’ tax reform package, which repealed Obamacare’s individual mandate when it went into effect Jan. 1, as a reason for the projected rising rates.
New York state’s Department of Financial Services noted that “insurers have attributed approximately half of their requested rate increases to the risks they see resulting from its repeal.”
But Haislmaier said only a small percentage of premium increases are due to Congress’ repealing the Affordable Care Act’s mandate for all individuals to purchase health insurance.
“The question then is to what extent does the individual mandate play a role,” Haislmaier said. “It is interesting that the insurers, in their submissions in New York, varied widely in that—everywhere from zero to [a] 25 percent rate increase.”
Insurance companies have attempted to cut costs at the expense of quality and choice, analysts say.
“Preferred provider organizations allow you to go to more doctors and hospitals; they have a wide network,” Haislmaier said. “One of the things that we have seen happen in Obamacare is to control costs, the insurers moved away from those plans to more restricted networks where you can only go to doctors and hospitals that take lower rates.”