How the GOP Can Make Graham-Cassidy a Success
Jean Morrow / Marie Fishpaw /
Over the weekend, Republican senators released a new version of “Graham-Cassidy,” their latest effort to undo Obamacare’s damage.
It’s far from clear the bill can get enough votes to pass, but negotiations continue behind closed doors.
Here at The Heritage Foundation, we have kept close track of the major bills Congress has considered to provide relief from Obamacare’s mandates.
Like the previous House and Senate health care bills and the earliest versions of the Graham-Cassidy bill, this version falls short of fully repealing Obamacare and replacing it with a patient-centered system.
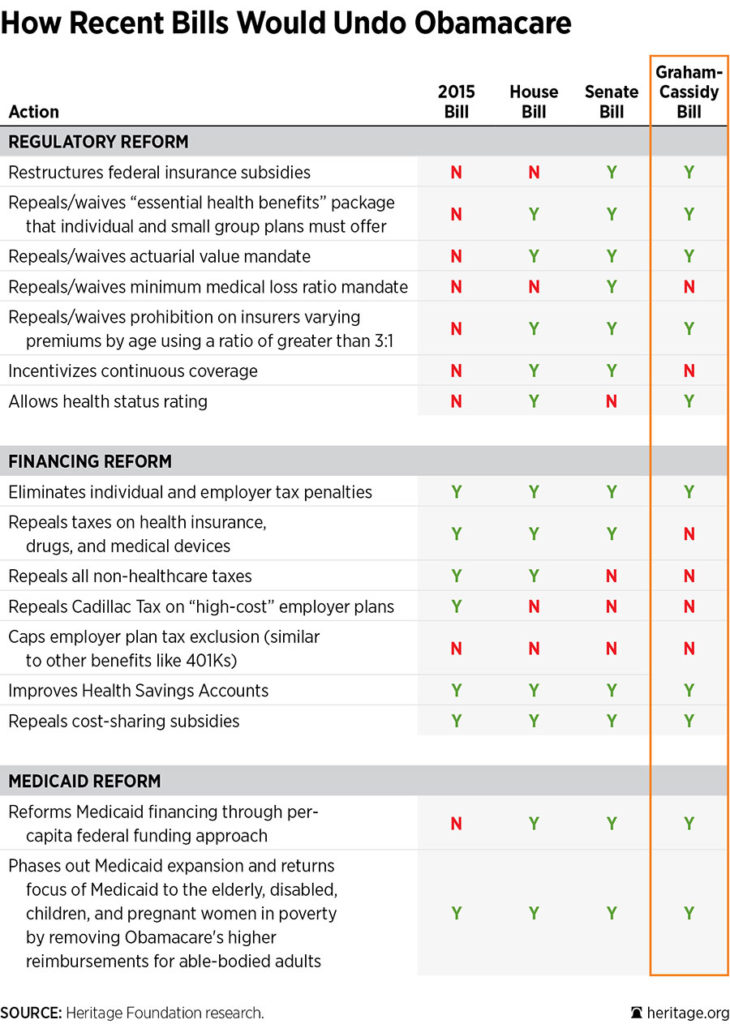
But as the chart below illustrates, Graham-Cassidy–so named after original Republican sponsors Lindsey Graham of South Carolina and Bill Cassidy of Louisiana–provides regulatory relief and gives states the ability to get out from under some of Obamacare’s most costly insurance mandates.
This latest version of the Graham-Cassidy bill also repeals the individual and employer mandate tax penalties in Obamacare and provides Medicaid reform. These provisions are good: As we’ve pointed out, it’s critical to free states from the Obamacare insurance mandates.
However, a significant concern that we previously noted remains in the current version of Graham-Cassidy.
Specifically, the block grant program in the bill is written such that states could use the money to simply expand government health programs. In the worse case, this could result in transferring up to 8 million people (half of the people in the individual market) from private coverage into government-run programs with no consumer choice.
To be consistent with the sponsors’ intent, the bill should be modified to ensure that any state using federal dollars to subsidize health insurance allows recipients to purchase the coverage of their choice in a competitive private market.
Maintaining and expanding consumer choice of coverage is the difference between a patient-driven system and a program that puts first the needs of providers and special interests.