More Research Refutes Efficacy of Masks Against COVID-19
S. Stanley Young / Warren Kindzierski /
As flu—and coronavirus—season approaches, Dr. Anthony Fauci is again saying that wearing face masks protects individuals from spreading the coronavirus.
Some colleges and hospitals are reinstating mask mandates.
Politics and the fear of coronavirus may have held sway the past few years, but common sense and rational science need to prevail now. Masks are ineffective, and mask mandates are unnecessary.
We offer several explanations from our National Association of Scholars report and peer-reviewed study to refute doomsayers’ warnings about the effectiveness of wearing masks.
Viruses Go Around, Through Masks
Coronaviruses are very small, with a size range of 0.06 to 0.16 micron. For perspective, 1,000 microns equals 1 millimeter. Respiratory viruses like the coronavirus are transmitted through secretion fluids during breathing in the form of small aerosols (less than 5 microns in size) or larger droplets (greater than 5 microns in size), rather than isolated viruses.
When viral-infected humans breathe, talk, eat, cough or sneeze, they emit aerosols and droplets containing viruses.
Aerosols emitted from simple breathing are small (size range 0.2 to 0.6 micron), and once emitted can be present in an enclosed setting for several hours. A person showing no symptoms of viral infection does not cough and sneeze, and therefore they do not emit large droplets.
Aerosols less than 0.5 micron are not easily filtered out of air by any physical mechanism. The openings in medical masks range from 0.3 to 10 microns in size. The latter dimension is much larger than small aerosols emitted from an infected person.
Now, there are a couple of ways in which virus-laden aerosols can infect a person wearing a mask when the aerosols are present in their breathing zone. One way is aerosol penetration through the mask during breathing because mask openings are too large.
A second way is breathing air containing aerosols from the side of a mask due to incorrect wear, increased mask resistance, or poor string tension. A mask wearer breathes out moist air, which increases mask resistance by plugging up the openings. Simple breathing has been shown to emit up to 7,200 aerosols per liter of exhaled air. While this can reduce aerosol penetration through a mask, it worsens the problem of inhaling virus-laden aerosols from the side of the mask.
Controlled Trials Show Masks Not Effective
The leading Cochrane Database of Systematic Reviews published a review in 2020 and a reanalysis in 2023 of human controlled trials using masks to slow the spread of respiratory viruses.
Both of these studies concluded that it is uncertain whether wearing masks help to slow the spread of respiratory viruses. Outside of the Cochrane organization’s influence, one of the senior authors of both studies (Jefferson) was more to the point: “There is just no evidence that [masks] make any difference. Full stop.”
Jefferson’s findings are consistent with viral transmission basics. Is he right? To answer this, we independently evaluated his data used in the 2020 review using a novel statistical p-value plot.
A p-value plot is used to visually inspect characteristics of a set of test statistics addressing the same research claim; for example, do masks make any difference? The plot is well-respected, being cited more than 500 times in the literature. The plot examined whether p-values support no association (randomness) or a real association between community mask use and viral infections.
Jefferson’s 2020 review looked at 15 separate community (that is, non-health care worker) controlled trials comparing medical masks to no masks. We took the results from these 15 trials—risk ratios and confidence intervals—and converted them to p-values.
The p-values were plotted according to rank (smallest to largest values). The plot is interpreted as follows:
- If p-values follow an approximate 45-degree line, the data set supports randomness (no association); that is, masks don’t work.
- If p-values approximately follow a line with a flat/shallow slope, where most of the p-values are small (less than 0.05), then the set of p-values provides evidence for a real association; that is, masks work.
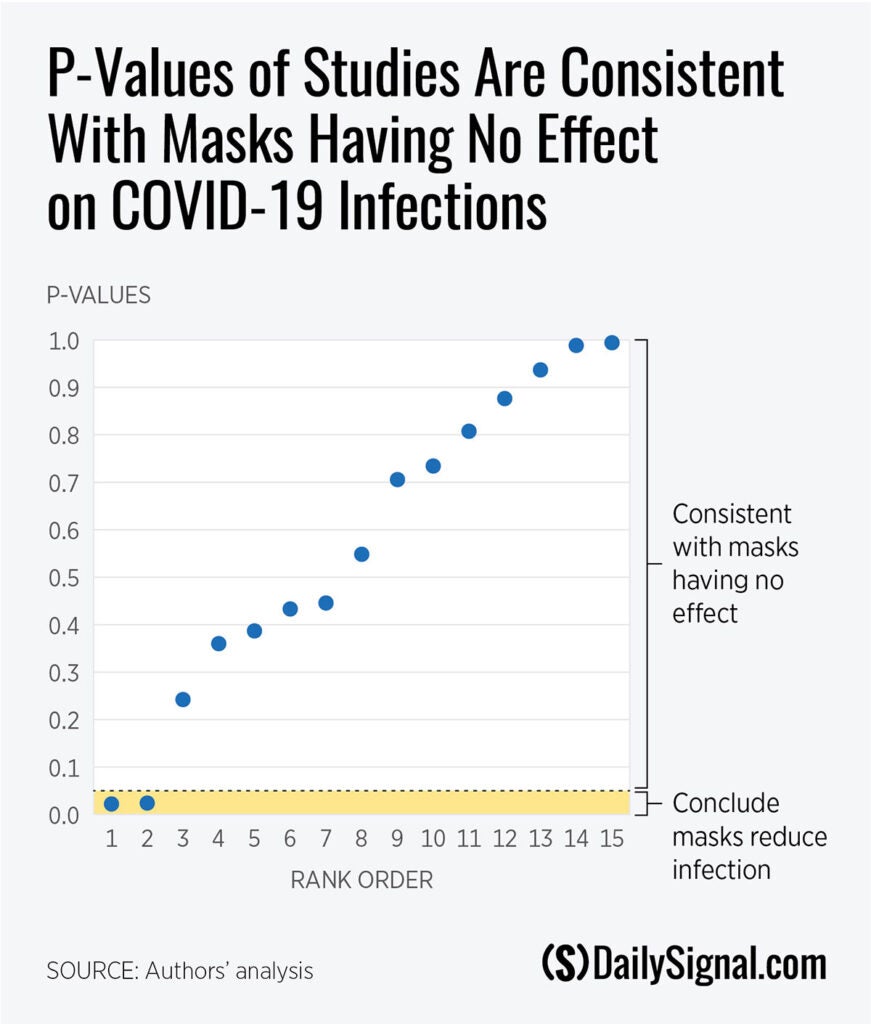
The p-value plot of the 15 controlled trials clearly shows p-values aligned approximately 45 degrees, indicating randomness. This is consistent with what Jefferson found: Masks don’t work.
A Natural Experiment Shows Ineffectiveness
A final explanation is a natural experiment of World Health Organization-reported daily new COVID-19 deaths in Germany and Sweden during the second wave (October 2020 through July 2021). At the time, Germany had a mask mandate, whereas Sweden did not, as they followed a strategy to let herd immunity develop naturally.
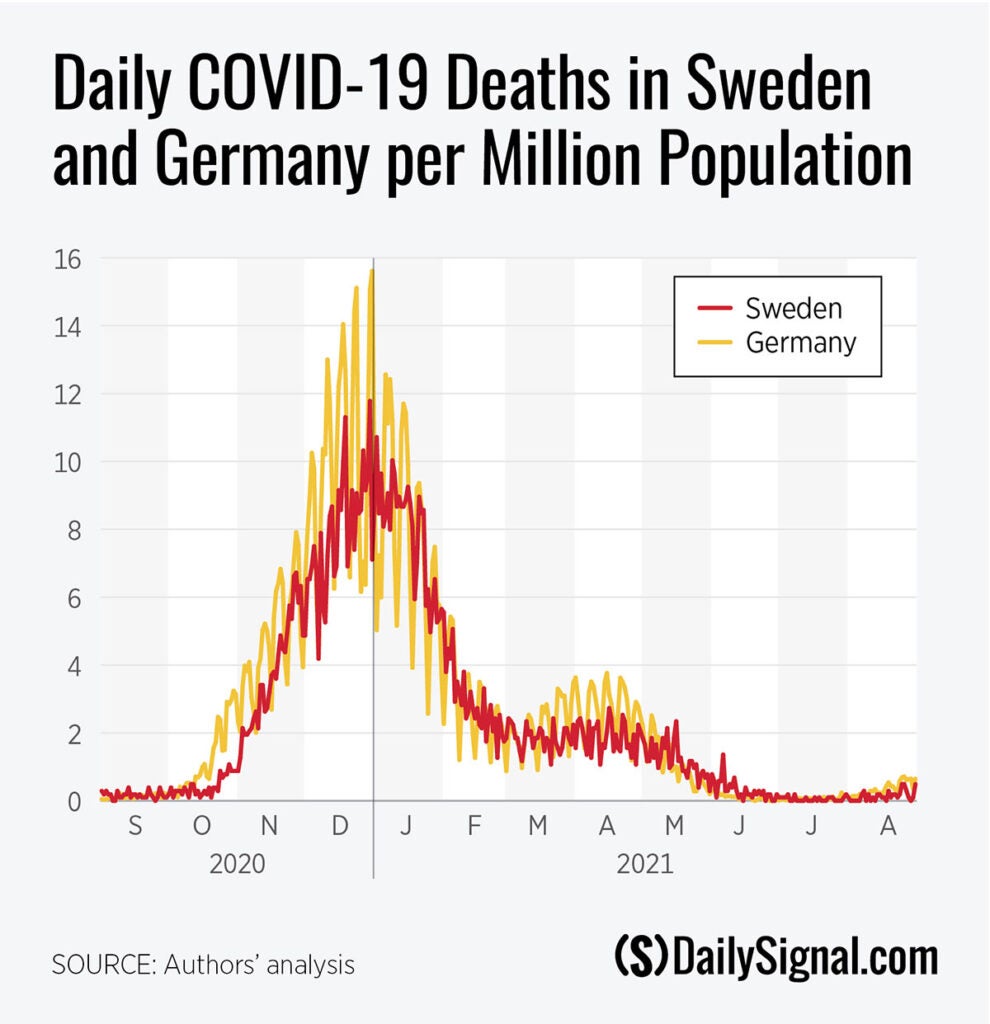
Many factors contribute to mortality risk. Numerous influences may be at play in the airborne respiratory virus-mortality chain across populations; for example, access to health care, health status, lifestyle, standard of living, etc., which complicates efforts to draw conclusions from observational data.
However, Germany and Sweden are members of the European Union with similar national health policies. Both should have had similar capacities to respond to the COVID-19 pandemic. Also, in 2020, Germany and Sweden ranked closely in the top 10 countries of the world with the United Nations Human Development Index: Germany sixth and Sweden seventh. So, comparing the two should control for many factors affecting mortality.
Moreover, mask wearing was very dissimilar in the two countries. Survey data on mask compliance during the pandemic was captured in many countries by the University of Maryland Social Data Science Center and Facebook. Using these data, we observed that monthly average mask compliance in Germany was never less than 80%, whereas in Sweden it was never more than 21%, during the second wave.
Those figures shows that mask use had little or no benefit in preventing COVID-19 deaths in Germany and Sweden during the second wave. Despite similar health care capacities, similar Human Development Index measures, and obvious differences in mask compliance for the two countries, daily COVID-19 deaths per million population were not much different.
Policymakers Should Learn From Experience
It is the obligation of those espousing a theory to provide solid supporting evidence. Undoubtedly, more studies on the medical maskrespiratory virus infection research question, including COVID-19, will be presented in literature in the coming years as those in favor of mask mandates look for empirical support.
However, the evidence to date offers no support for mask mandates.
While research continues, experience and common sense can serve as a complement to the existing empirical results. An old-timer told one of us (Kindzierski) that he spent almost 40 years in the grain industry in Canada. He got used to using N95 masks to protect against grain-dust exposure. He said it used to state on the boxes containing the masks: Not effective against viruses.
Masks didn’t work then, and they don’t work now, to slow the spread of respiratory viruses. Full stop.
The Daily Signal publishes a variety of perspectives. Nothing written here is to be construed as representing the views of The Heritage Foundation.
Have an opinion about this article? To sound off, please email letters@DailySignal.com and we’ll consider publishing your edited remarks in our regular “We Hear You” feature. Remember to include the url or headline of the article plus your name and town and/or state.
