BETHLEHEM, N.H.—They came to be addicted to drugs in different ways, but ended up in the same place.
Steven Blaisdell, 26, a stocky, shy son of a mailman, was first prescribed pain medicine—the opioid OxyContin—as a teenager after he flipped over his four-wheeler and broke his left femur in half.
Over the past 14 years, Blaisdell has had surgery seven times as a result of recreational injuries that are common here in “North Country,” where young men treat the outdoors—mountains, ski jumps, and hiking trails—like a playground.
Part 2 of 5: One Opioid Addict Helps Another Choose Life Over Death
When he sits down, Blaisdell’s left shoulder droops lower than his right, dragged down by a 9-inch plate, the result of a dirt bike accident.
Blaisdell says his pain went away when he took up to 15 OxyContin pills per day, much more than he was prescribed.
After doctors stopped prescribing him the painkiller, Blaisdell—21 years old at the time and arthritic from repeated physical trauma—turned to heroin, a cheaper, illicit opioid, smoking it instead of injecting it because he’s scared of needles.
“From the time I was 13, doctors were pushing me pain pills as a safe alternative,” Blaisdell tells The Daily Signal four days after he relapsed on heroin over the Easter holiday, ending his latest attempt at sobriety. “I was prescribed pretty high amounts of them for a long time. I didn’t really have a lot of education growing up or warning about addiction until I was already addicted. So that’s kind of how it started for me.”
Moses Henry, 35, small in stature and blunt in speech, with body tattoos and face piercings, says he sought out drugs to fit in with friends.
Henry started with pot at 12 years old, graduated to cocaine at 15, and became addicted to OxyContin by the time he was 18, attracted to the stronger high and ease of purchase on the streets.
“I wasn’t in pain,” says Henry, who nearly died after he overdosed in the bathroom of his parents’ house over a year ago. “Drugs brought me up. I could do anything I wanted to do on OxyContin, on opioids. I am my own worst enemy.”
On just another foggy, gray late April day in northern New Hampshire, Blaisdell and Henry sit next to each other at a picnic table inside the poorly lit kitchen of a dilapidated, secluded cottage. This is the region’s only residential drug treatment center.
Friendship House, as the place is called, is where Blaisdell and Henry took themselves before it was too late.
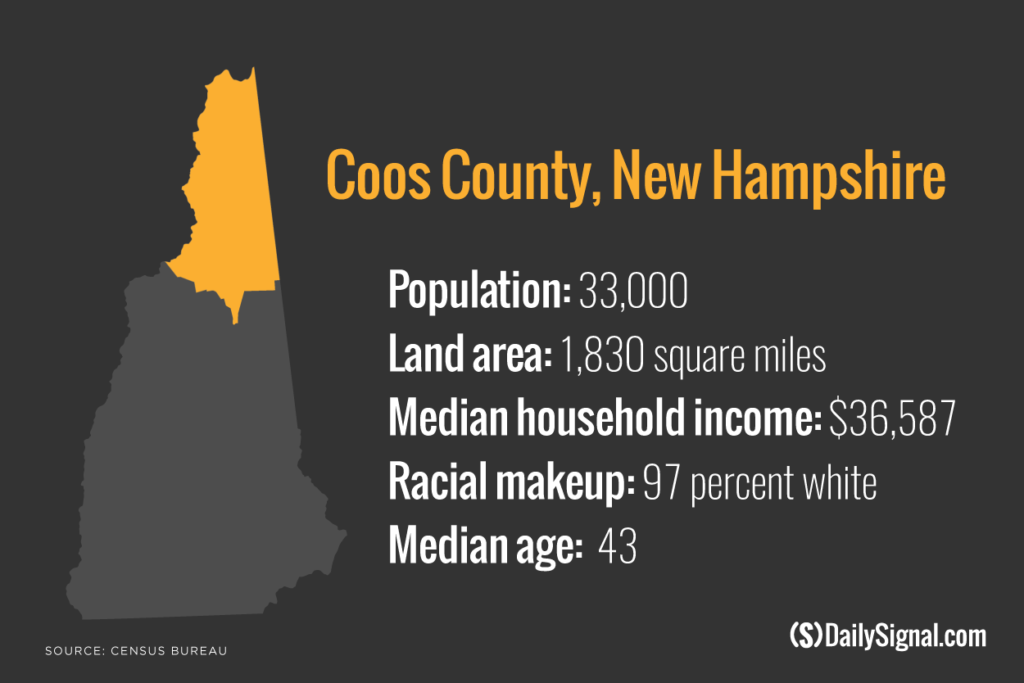
Blaisdell and Henry are both from Coos County, which has the highest combined death rate due to drugs, alcohol, or suicide in all of New England, comprising counties in six states.
The death rate is defined as the number of drug-related, alcohol-related, and suicide deaths per 100,000 people.
Coos County, New Hampshire’s poorest, also is the state’s largest county by land mass but smallest according to population.
Driving through the county’s numerous tiny and nearly deserted towns, where cellphone service becomes scarcer as a visitor creeps north—closer to the Canadian border—it’s difficult to appreciate how anybody could know anybody, because there doesn’t seem to be anybody living here.
A recent senior class at Pittsburg High School, in Coos County’s northernmost town, graduated one person.
But many of the county’s 30,000 residents are related by drug addiction, familiar with the region’s—and nation’s–opioid epidemic in some way.
“I can spot another addict from a mile away,” Henry says, motioning a couple feet away to his right, at Blaisdell. “You try to escape it, but it’s hard.”
In Recovery, ‘Short Window of Opportunity’
Blaisdell and Henry are in the same residence, but at different stages of recovery.
Henry is employed as a “recovery coach” at Friendship House, where he became sober 14 months ago as a resident here. He is mentoring Blaisdell, who is voluntarily participating in a 90-day, low-intensity residential treatment program, designed to support drug users in the early stages of recovery.
This series:
Part 1: The Crisis That May Have Swung Voters From Obama to Trump
Part 2: One Opioid Addict Helps Another Choose Life Over Death
Part 3: ‘Dr. Father Pill’ Wants to Be Part of the Solution
Part 4: Police Assault on Opioids Gets Boost From a Family Doctor
Part 5: The First Responders Who Witness a Dreadful Toll
Serving New Hampshire’s three most northern counties, including Coos, Friendship House offers individual and family counseling, group therapy, and a place to live in a structured setting.
Many of the residents are homeless before they come here. Blaisdell and Henry both have been homeless at points of their addiction.
The facility, a one-story, wood-frame building in a wooded area that looks like a camp site, is not up to code and has only 18 beds. That’s not enough to serve the Northern Country, the upper third of New Hampshire, says Friendship House’s director, Kristy Letendre.

Kristy Letendre, Friendship House’s director, says “there is a short window of opportunity” to help opioid addicts recover when they seek treatment. (Photo: Josh Siegel/The Daily Signal)
New Hampshire has the second-lowest level of access to substance abuse treatment in the nation, above only Texas, according to the U.S. Substance Abuse and Mental Health Services Administration.
Friendship House is a part of the Tri-County Community Action Program, a nonprofit that also offers services to the homeless, elderly, and victims of sexual and domestic abuse.
Letendre says Friendship House recently received a federal Community Development Block Grant to construct a new building that meets code requirements and will allow the center to expand to 32 beds. As part of that expansion, the Tri-County Community Action Program recently merged with North Country Health Consortium, a similar nonprofit provider.
Letendre says growth is necessary because she regularly has to turn down drug addicts who want to stay at Friendship House, with individuals facing a wait time that can span four to six weeks.
That delay could be too long to make a difference.
“There is a short window of opportunity when you are talking to somebody who is ready to give up using,” says Letendre, a hard-charging 38-year-old who wears dangling earrings and a jean jacket.
“If they make a call to you at that point, they are hopeless, they have burned every bridge, and they are going to die if they continue to use,” Letendre adds, pounding a table for emphasis, her wrist jewelry clanking:
If they pick up the phone and call me, if I can bring them right in, I have a chance to save that life. If I can’t bring them in, and have to tell them they have to wait to get into treatment services, at that point they lose hope. ‘No one cares about me, I don’t care if I live or die.’ You are playing Russian roulette. So they go out and use, and when they use, that is when you see the overdose.
‘Easier to Die’
Henry says he became committed to recovery after overdosing for the seventh—and latest—time in January 2016.
He was revived by his father, who gave him CPR for seven minutes on the bathroom floor of the family home before the ambulance came.
“That look in his eyes really destroyed me,” Henry says of his father, who before this most intimate of moments had not been on speaking terms with his son. “I don’t know what he said to me. I can tell you what I said to him. I asked him where my drugs were and why did you even bother reviving me. Because it was easier to die at that moment. It was the easiest way out. I didn’t want to do what I needed to do to get sober. Because it’s hard work. It was easier to just give up on everything.”
As his parents drove him to Friendship House from their home in Berlin, Coos’ only city, Henry says he injected a gram and a half of heroin.
Henry had been to Friendship House once before, eight years ago now, but quickly relapsed after he detoxed.
“I am an addict, and I’m sorry,” Henry says. “It didn’t work out the first time, but I didn’t put any effort into my recovery.”
He says he was inspired to recover after he read a handwritten letter by his 14-year-old niece, Padence, who calls him Uncle Mosey.
In the letter, which Henry provided to The Daily Signal, Padence writes that she feared her uncle “would die before I was able to have him in my life again.”
Padence has seen Henry high on drugs.
“I never truly had my uncle in my life for my whole life,” Padence recalls, in neat handwriting and flawless spelling:
I got to have him for a little while. But I never held on too much cause I would always lose him again. Because I love him, it was hard. After a while, I couldn’t stand seeing him. I never hated him, but I hated the things he did and who he became.
At his lowest points, Henry took 10 grams of heroin a day, he says, and stole from his parents and grandparents to feed his drug addiction. It was a stark fall.
He had lived a middle-class childhood provided by his father, who worked in a paper mill before the industry dissolved over the past 20 years. He says his parents never drank or used drugs.
Henry says he started and ran his own carpentry business for eight years, claiming that he made six figures at 18 years old.
‘It Gets Easier, but Harder Too’
Today, Henry aspires to go to college to become a drug and alcohol counselor, and he’s here to articulate to Blaisdell the challenges of recovery.
This is also Blaisdell’s second stay at Friendship House.
The first time, he remained sober for an intensive 28-day program, where he detoxed off the opioid drugs.
But shortly after leaving, Blaisdell relapsed, using heroin on Easter to escape from family pressures, he says.
“He didn’t fail,” Henry says reassuringly of Blaisdell, who was living in a homeless shelter at the time of his relapse. “It’s a speed bump. I told him don’t beat himself up over it. It does happen. It’s hell. Addiction is hell. What he’s going through—it gets easier, but it gets harder too.”
Blaisdell says he’s in a better position to stay sober now that he has detoxed once and experienced the symptoms of withdrawal.
“The best way I can describe it is to say it’s like when you are very hungry or very thirsty and it just takes over your mind and it’s all you can think about,” Blaisdell says. “Where am I going to get my next meal, where am I going to get my next dose [of drugs]? Getting the next dose is really all you think about. The opioid withdrawals are so intense that you become quite fearful when you go through it.”
Letendre says Blaisdell’s experience is typical for an addict. Repeated use of an opioid, she says, can alter an individual’s brain chemistry and lead to physical and psychological dependence.
Opiates change the way the brain responds to pain and can produce a “high” feeling, disrupting the brain’s reward and pleasure centers. Without the drug, the body may not feel what it learned to know as normal, leading to withdrawal symptoms such as sweats, muscle aches, vomiting, and diarrhea.
“When our body builds this physical dependence, the withdrawal is severe and immediate,” Letendre says. “The user will do everything they possibly can to get the money to get their fix.”
‘Keep Up His Habit’
While Blaisdell says he chose on his own volition to come to Friendship House to get better, his experience here may have an outsize impact on his future.
In September 2016, according to court records obtained by The Daily Signal, Blaisdell was indicted in Coos County Superior Court on multiple felony charges of selling heroin and fentanyl—a more powerful synthetic pain medication—and engaging in a conspiracy to sell drugs.
Blaisdell made $10,000 bail—paid by his father—and has a pretrial hearing scheduled for September.
His court-appointed attorney, Joseph Garrison, says Blaisdell sold drugs to a state police officer who was undercover.
Garrison, in an interview with The Daily Signal, says Blaisdell told him he sold drugs to make money to feed his own addiction. In New Hampshire, Garrison says, Class B felonies, with which Blaisdell has been charged, are punishable by a maximum sentence of three to seven years in state prison.
“Unfortunately, Steven’s situation is far too common right now,” Garrison says. “He became addicted, and based on my understanding, it was one of these things where he was trying to keep up his habit. He’s not big time. He’s not like a giant dealer. It’s more a personal-use type situation. He’s a really nice guy who just has a really severe drug problem.”
Garrison, who represents clients in New Hampshire’s three northernmost counties—Coos, Grafton, and Carroll—says half of his caseload involves drug-related offenses. [Note: When first published, this report incorrectly said Groveton rather than Grafton.]
He advises clients such as Blaisdell to seek treatment before trial to show they want to overcome their drug problem.
“I have too many of these cases,” Garrison says, adding:
I have clients who overdose and die before trial. I have had clients go out and commit more crime. Steven is taking this to heart, which is a huge silver lining in the case. Our hope is we can keep that going so he stays sober and makes better choices in the future.
Blaisdell, for his part, acknowledges to The Daily Signal that he is charged with drug-related crimes, although he does not admit directly to selling drugs.
“What most people don’t realize is that a lot of the dealers are addicts themselves and they are just trying to get by,” Blaisdell says.
He insists his ambition to fulfill Friendship House’s treatment program is genuine, and not just about looking good for court.
“I want to get better,” Blaisdell says. “That’s why I am here. Can I imagine going back to drugs? I can imagine it, but it’s absolutely not what I want. This addiction has taken my independence from me. It’s ruined every relationship I ever had. I am now just starting to make amends with my older sisters and getting my family back—and my life. You become very selfish. I’m always one of the last people to ask people for help. I always wait until it’s either too late or close to it.”
Letendre, the Friendship House director, knows about Blaisdell’s criminal charges. She says she’s had plenty of residents who’ve relapsed during their path to recovery, and she didn’t consider Blaisdell’s recent slip-up in deciding whether to give him another opportunity.
She says without treatment, Blaisdell—facing prison time—could experience a worse outcome.
“When a person says, ‘I need help to save my life,’ absolutely they are usually ready,” Letendre says. “If I can’t that first time, I hope that second time I can help.”
‘Hope in a Small Rural Community’
For addicts in the North Country, the path to get better is especially steep, because the reminders—and temptations—of drug abuse are so close.
“I know a lot of people in active use,” Henry says. “You know, I have buried seven or eight friends in the past year. Two brothers OD’d within a week of each other. That mother buried two kids within two weeks.”
Despite the bleakness around them, Blaisdell and Henry say they want to spend the rest of their lives in or near Coos County. They see beauty where others see economic struggle and pain.
“North Country has a lot of resilience,” Henry says. “I love the outdoors, I love the four seasons.”
To find fulfillment in Coos County and live drug-free, Henry and Letendre advise Blaisdell to strive to make new friends, to form a peer group of sober-minded people like he has at Friendship House.
“Moses [Henry] is the hope in a small rural community,” Letendre says, explaining:
If you are going back to a community that has nothing but your old dealers, what are you going to do? How are you going to change your friends? How are you going to make connections? You need to have a safe place—strong support when you go home.
Addiction is like chronic illness. It’s never going go away. There is no cure for it. All we can do is provide support, provide education. A person can be successful when that person has everything in place for them. Relapse is inevitable unless those supports are in place.
Blaisdell says he is on good terms with his parents, after years in which they refused to speak with him.
“I believe my family is 100 percent supportive of me being here,” Blaisdell says. “If they aren’t willing to accept me, all I can do is the best I can. If they aren’t willing to accept my apology, I just got to move on or maybe try again.”
Currently unemployed, Blaisdell says he wants to return to working as a mechanic. In high school, he says, he earned certification for state inspections, although he struggled to hold down related jobs because of his addiction.
At Friendship House, Blaisdell takes out the trash and cleans toilets.
“It’s good to know I can do the job and know it’s done right,” he says. “I live here, and want it to be clean and sanitary.”
Friendship House prescribes chores to instill discipline and ownership as part of recovery.
It’s a sort of return to childhood—before the drugs—that Blaisdell says he embraces.
“The drug lifestyle leads nowhere,” Blaisdell says. “It just brings pain and eventually death. A lot of addicts know that, but they are just scared to give it up. I figure if I put half the effort into being sober as I did being an addict, I know I can do it.”
Next, in Part 3: Meet the doctor who helped create the local opioid addiction crisis, and see what he’s doing to help solve it.